
F
How novel approaches and partnerships could help to address capacity issues for Pelvic Floor surgery
Mohammed Belal, Hashim Hashim, Wesley Lai, Charles Maxwell-Armstrong, Charles Knowles (editor)
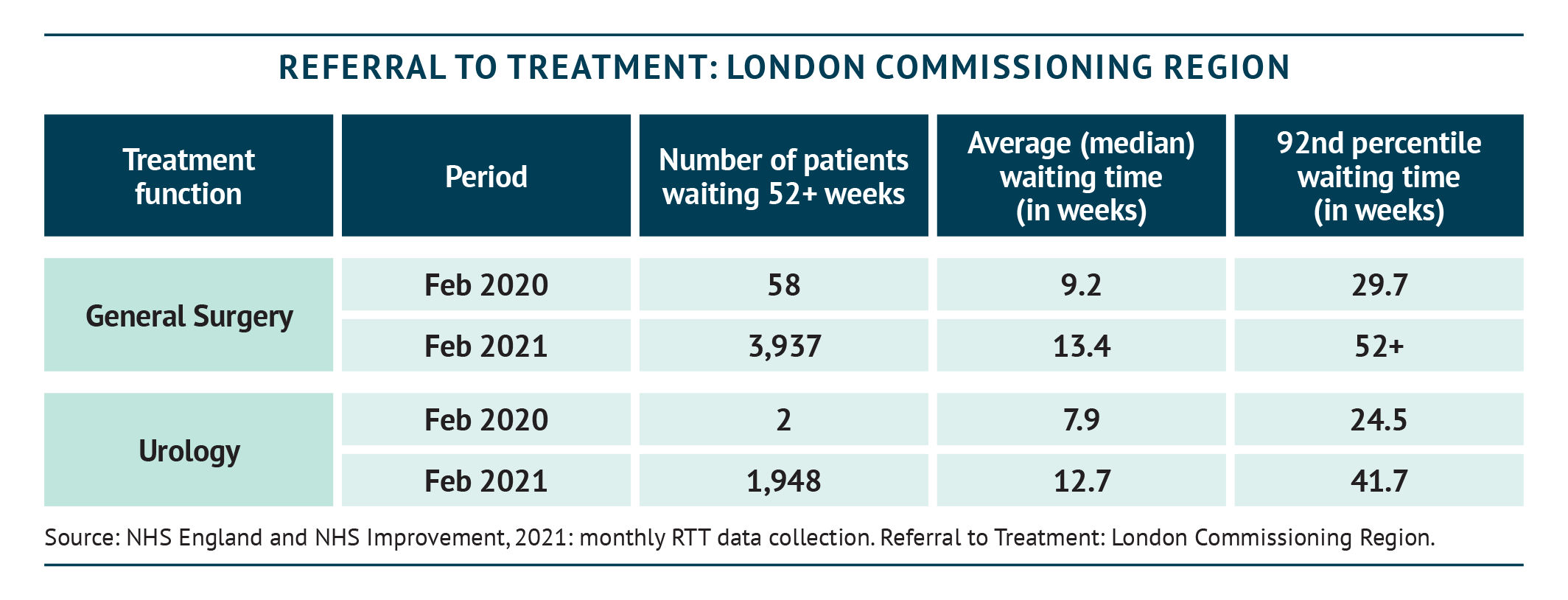
Waiting lists for pelvic floor procedures, classified as ‘benign work’, are always lengthy, but have been worsened by the recent COVID-19 crisis. The pandemic led to a hold on all non-urgent procedures (diagnostic and surgical), which has seen waiting lists for pelvic floor procedures grow to 400 –500 people in some large NHS Trusts. By February 2021, nearly 388,000 patients across all therapy areas in England had been awaiting routine hospital treatment for over a year (BBC, 2021). The numbers of patients waiting for 52 weeks for general surgery and urology surgery in London alone are shown in the table below – these include patients with problems deemed ‘less urgent’ (including pelvic floor issues).
Pressures on benign procedures during the COVID-19 era have come from multiple sources, including the delays to cancer assessment and care, with about 38,000 fewer cancer treatments taking place between March and July 2020 (Cancer Research UK, 2020). This leaves a backlog of potential cancer patients, that needs to be cleared, and will always take priority over benign pelvic floor pathology, even though pelvic floor problems have a significant physical and mental impact on the patient. Other non-oncology departments are also competing for the same limited hospital resources in the post-COVID-19 period, and many, such as trauma patients, may also take priority over pelvic floor patients. Finally, in addition to the normal ‘winter pressures’ on beds, ring-fencing of ‘COVID beds’ has further reduced hospital capacity for elective inpatient procedures.
This is likely to increase with further waves of COVID-19. With a lack of surgical space and theatre time for pelvic floor surgery, creative solutions and partnerships with other providers are worthy of consideration.
Public-private initiatives have always been controversial in the NHS in the past, with both positive and negative experiences. The panel does not endorse any particular model, but does feel it is important to look at the pros and cons of different approaches within a fully integrated pelvic floor service.


KEY POINTS
- Private institutions and premises may be able to support specific challenges, particularly in addressing growing waiting lists
- New approaches, whether these are use of private resources or mobile units, could be particularly suited to day cases owing to their use of sedation and short patient stays
- The off-site nature of private providers aligns with the concept of pooled regional activity from several trusts
- Challenges relating to the private sector must be carefully considered, including care delivered by the same team, patient selection, maintaining quality of care and prevention of conflict of interest issues
Considering collaboration: a potential new approach
While COVID-19 has contributed to the waiting list challenge for pelvic floor surgery, experience gained during the crisis may also offer insights into ways to tackle this challenge. In fact, public-private collaboration in the pelvic floor sphere had been trialled before the pandemic (Chard et al., 2011), but these became a common feature during the initial COVID-19 peak in the spring and summer of 2020. Private hospitals in many areas have been used for benign and cancer cases since the pandemic began to peak around April, providing ‘green sites’ for patients vulnerable to infection. However, while there have been positive experiences with these collaborations, in many areas there were also logistical issues and problems with efficiency. Treatment centres may provide an alternative to private hospitals, but consideration must be given to the provision of specialists and specific equipment required.
Private institutions may be able to help with specific challenges. An obvious use would be to address very long waiting times in the NHS for particular procedures. Using private resources, such as theatres, could make the most of available capacity in local private institutions when capacity is at a premium within the NHS. Private facilities could help to reduce waiting lists on the NHS, potentially also offering services during evenings and weekends to further address the backlog.
However, this is only one driver for change. The private sector is also an opportunity to improve quality and patient experience. Some busy acute hospitals make for poor environments to ‘squeeze in’ elective pelvic floor cases, especially when the mindset of staff is on other priorities.
Pelvic floor procedures that can be performed as day-case surgery are an obvious choice for public/private partnerships. Sacral neuromodulation (SNM) is an example of a procedure that may be suited to a private hospital or treatment centre. SNM cases are day cases, with patients under local anaesthetic (see Chapter D), sedation or general anaesthetic and in and out of hospital quickly, and SNM is a minimally invasive approach. Day-case units have been established in multiple NHS Trusts in the past, and could once again be worthy of more attention as a concept.
There is a rationale to pool patients on dedicated lists, run for a single region by one provider with the infrastructure to deliver this without interruption and to adhere to the critical time sequence for the SNM stages (SNM requires two sequenced procedures a few weeks apart). Other procedures that could benefit from this approach include injectables or proctology procedures, such as haemorrhoids or simple fistulae.
An alternative approach for these procedures is mobile units, which can travel around the country to provide extra facilities and specialist equipment. These might provide an additional route to reducing overload, though logistics and requirements may vary from Trust to Trust. A further option could be to locate nurse-led clinics in the private sector but to maintain day cases within the NHS itself, or indeed to develop purpose-built temporary operating theatres – an approach trialled in some places before the pandemic (BBC, 2019).


CASE STUDY: NOTTINGHAM UNIVERSITY HOSPITALS NHS TRUST COLLABORATION WITH CIRCLE
A collaboration between Nottingham and Circle provided the ability to move the pelvic floor service between sectors, maintaining the service while the NHS was under pressure. The collaboration ended shortly before the onset of COVID-19, with waiting lists reduced to manageability by the collaboration and the NHS now back in control.

CASE STUDY: UNIVERSITY HOSPITALS PLYMOUTH NHS TRUST
The Plymouth Pelvic Unit and UHP have been in ongoing discussion with the local independent sectors with a plan to move some of the pelvic floor procedures such as perineal rectal prolapse repair and SNM to their sites, in order to help with the growing waiting list, especially during the COVID-19 pandemic. In January 2021 NHS Improvement (NHSI) triggered the ‘Surge’ clause in the national contract, and the pelvic floor team has successfully performed selected pelvic floor procedures such as perineal rectopexy and SNM in the Nuffield hospital Plymouth.
Anticipating and overcoming challenges
While there are clear potential benefits, the challenges of public-private collaboration must also be considered. For example, more complex procedures that require a large team, overnight stays and detailed follow-up may be problematic if performed at a location miles away from where the experts are located. COVID-19 has highlighted this challenge when individual consultants have on occasion found themselves split across multiple sites, many miles apart, to ensure patients were covered. While this might be achievable during a crisis, it is not sustainable in the long term.
In fact, even for a day-case procedure, patient assessment and follow-up must be considered. These assessments involve a multidisciplinary team of nurse specialists, radiographers and clinical scientists as well as the surgeon. Any public/private partnership needs to consider this complexity, and not simply whether the institution has the surgical space and equipment to perform the procedure. It may be that a blended approach is appropriate – with non-NHS institutions providing the facilities for surgery, but with the pre- and post-care of the patient taking place within NHS outpatient facilities, with decision making passing through regional MDTs (see Chapter C and Chapter E).
The use of private facilities may be best suited to the fittest (ASA1 and 2) patients, to minimise the risk of complications that would be better handled in an NHS centre. Further, while capacity may be available in the private sector, it is not geared up to handle the numbers of patients passing through the NHS, and consequently private hospitals may be less willing to take on patients in the future outside the current crisis period. We must not ignore that public and healthcare professional (HCP) discomfort, with the idea of private involvement in the NHS, may raise additional barriers.
Maintaining the quality of patient care
Above all, at all times, quality is critical. Whatever the approach taken, a quality agenda will be required to ensure standards are maintained and previous negative experiences of public-private partnerships (House of Commons Health Committee, 2006; Royal College of Surgeons, 2006; Plumridge, 2008; BBC, 2015; Cumberlege Report, 2020) are not repeated.
Perhaps looking at public/private partnerships – carefully developed – could be one option to address the large waiting lists that now exist for patients with pelvic floor problems. The COVID-19 experience is teaching us that we are able to find solutions to challenges where there is a will. While there is no single answer to the overload on PF services, an openness to collaboration and new ways of approaching the service may lead the way to identifying more sustainable models in the future.
REFERENCES
BBC, 2015. Hinchingbrooke Hospital: Circle to hand back to NHS by end of March. Available at: https://www.bbc.com/news/uk-england-cambridgeshire-31104003 (last accessed September 2020).
BBC, 2019. Hairmyres Hospital sets up ‘car park’ operating theatre. Available at: https://www.bbc.com/news/uk-scotland-glasgow-west-50573218 (last accessed October 2020).
BBC, 2021. 4.7 million waiting for operations in England. Available at: https://www.bbc.co.uk/news/health-56752599 (last accessed April 2021).
Cancer Research UK, 2020. One third of cancer patients say coronavirus has impacted their treatment. Available at: https://www.cancerresearchuk.org/about-us/cancer-news/news-report/2020-07-28-one-third-of-cancer-patients-say-coronavirus-has-impacted-their-treatment (last accessed October 2020).
Chard J, et al., 2011. Outcomes of elective surgery undertaken in independent sector treatment centres and NHS providers in England: audit of patient outcomes in surgery. Br Med J 343:d6404
Baroness Cumberlege, 2020. First Do No Harm: The report of the Independent Medicines and Medical Devices Safety Review. Available at: https://www.immdsreview.org.uk/Report.html (last accessed September 2020).
House of Commons Health Committee, 2006. Independent Sector Treatment Centres: Fourth Report of Session 2005–06. Available at: https://publications.parliament.uk/pa/cm200506/cmselect/cmhealth/934/934i.pdf
NHS England and NHS Improvement, 2021. Monthly RTT data collection. Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/ (last accessed April 2021).
Plumridge N, 2008. Running out of steam? Public Finance. Available at: https://www.publicfinance.co.uk/2008/05/running-out-steam-noel-plumridge (last accessed October 2020).
Royal College of Surgeons, 2006. Inquiry into independent sector treatment centres. Ann R Coll Surg Engl (Suppl) 88:116–119.